What should you do when an emergency room patient starts rapidly declining? How do you tell someone they have cancer? Do you know how to help calm an agitated patient? When is it time to reach out to the attending physician for help?
These are the kinds of questions that tens of thousands of new doctors across the United States will face this summer as they enter their first year of residency.
Yet it may have been months since they last practiced some skills, and they may have mostly observed others.
That’s where Transition to Residency (TTR) courses — commonly called TTR bootcamps — come in. Often held for two weeks toward the end of medical school, these intensives allow students to practice hands-on procedures, refine communication skills, boost confidence, and shift from a student to a practitioner mindset.
“There’s a huge jump in responsibility from being a medical student to a resident, so this can be one of the more problematic points in training. Our job is to make sure residents are ready on Day 1,” says Matthew Rustici, MD, who co-leads the TTR course at the University of Colorado (UC) School of Medicine in Aurora.
The number of TTR bootcamps has been climbing. Today, 90% of U.S. medical schools provide the courses, according to an AAMC survey, and the vast majority of schools require students to take them. A decade and a half ago, fewer than 20 such courses existed.
“There’s a huge jump in responsibility from being a medical student to a resident, so this can be one of the more problematic points in training. Our job is to make sure residents are ready on Day 1.”
Matthew Rustici, MD
University of Colorado School of Medicine
In 2021, the Coalition for Physician Accountability, which includes the AAMC and more than 10 other groups, issued key recommendations to improve the transition from medical school to residency. Among them was a call for TTR bootcamps, particularly those that offer a specialty-specific focus.
But running bootcamps is no simple matter, requiring a large cadre of instructors who can provide individualized feedback. They’re also not simple for students, who may be scrambling to move or trying to fit in personal milestones such as getting married before the rigorous residency years begin.
Still, bootcamps are worth the effort, advocates argue. “It’s a difficult, exhausting month here, but many of our students say it’s the best course they’ve taken in medical school,” says Rustici.
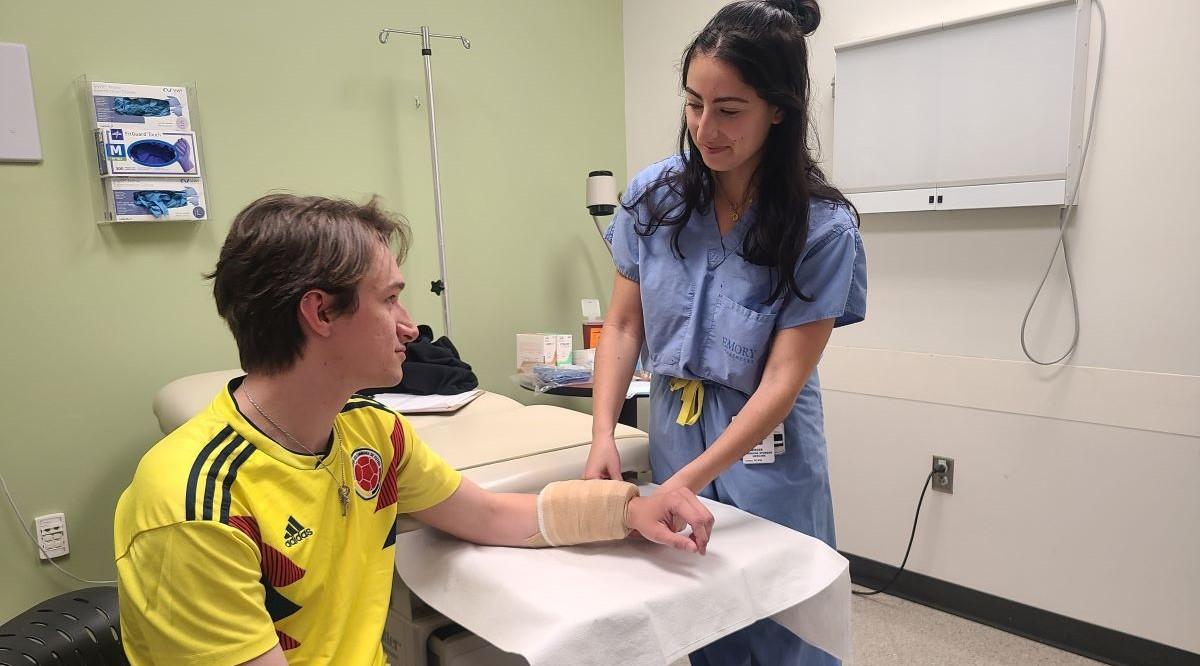
For Lara Schwieger, a fourth-year student at Emory School of Medicine in Atlanta, a key bootcamp benefit was increased peace of mind. “As a medical student, we are constantly observed. But as a resident you’re often on your own without direct supervision, which can be daunting,” she says. “I feel much more comfortable starting residency now that I’ve had the chance to practice skills I’ll be using day to day.”
Gearing up for the front lines
Medical students spend four intense years studying science and clinical care. So why do they need a bootcamp too?
It’s partly because though students may have observed or contributed to a medical process — like managing patient pain — they haven’t yet been frontline decision-makers. Plus, they haven’t had to handle patient care in a fast-paced, stressful environment — often with little sleep.
It’s also partly because of how medical education has evolved, experts say. “Compared to years ago, increased caution around patient safety has curtailed students’ ability to practice certain procedures,” says Keith Delman, MD, who oversaw Emory’s TTR bootcamp for a decade.
So bootcamps focus on actionable guidance, like when to suspect a lab error is causing abnormal results. They also rely on small-group exercises assessing common patient complaints. Often, they do so in tracks focused on specific medical fields.
But at the heart of any high-quality bootcamp are re-creations of real-world scenarios and hands-on practice in frequently used skills.
“I practiced placing and removing staples from a latex pad, inserting breathing and feeding tubes into manikins, and other common procedures. Being able to risk making mistakes in a simulation was so reassuring,” says Schwieger.

Students practice evaluating a critically ill patient during the Transition to Residency course at the University of Virginia School of Medicine.
Courtesy Life Support Learning Center, University of Virginia Health System
Bootcamp simulations can be quite realistic. For example, some medical manikins emit breathing sounds, have a pulse, and can even answer questions thanks to an instructor’s remote microphone.
At New York University (NYU) Grossman School of Medicine in Manhattan, one simulation replicates a medical emergency, replete with trained actors portraying family members and hospital staff. “Students are quickly reading test results, looking at scans, and talking to nurses. They are calling on information they learned in medical school and applying it to managing a patient’s care,” says Abigail Winkel, MD, who has helped run NYU’s bootcamp.
At the University of Texas Medical Branch (UTMB) in Galveston, one simulation covers a skill that’s needed from the outset of residency: how to answer a nurse’s page. For one week, students carry pagers and answer mock patient-care questions from nursing school students. “Hardly any of the students had used a pager before, and after the exercise, a survey showed a 30% increase in their confidence in handling pages, including using the pager and managing patient care over the phone,” explains Sidra Qureshi, MD, an assistant professor in internal medicine who codirects the course.
Beyond gaining necessary skills, a confidence boost is itself valuable, experts say, since feeling uncertain can undermine residents’ emotional well-being.
“Every year, when we start our simulations, we have some students standing uncomfortably at the foot of the bed, and by the end of the course, we throw out, ‘The patient presents with chest pain and low oxygen,’ and they shoot back, ‘Let’s get an EKG, chest x-ray, vital signs, and oxygen’,” says Kathryn Mutter, MD, MPH, who runs a bootcamp at the University of Virginia School of Medicine in Charlottesville. “It makes us proud.”
The human side of medicine
Being a doctor is about much more than procedural abilities. It’s also about the softer side of medicine.
In fact, surgery program directors who were asked what they wanted from bootcamp courses often highlighted skills beyond technical ones. “They said, ‘We can teach residents how to sew, but we want them to come in with communication skills, professionalism, and the ability to work in teams,” says Delman.
Communications lessons range from leading an informed consent conversation to sensitively delivering difficult news. At UC, students also practice how to respond compassionately when a patient asks for additional opioids for pain but providing such pain relief isn’t appropriate. “The goal is to avoid sounding judgmental,” says Rustici. “A provider might say, ‘I’m sorry you’re in so much pain, but considering opioids’ potential harm, we need to come up with a different plan.’”
Some courses also prepare students to speak up when a patient acts badly. Those lessons might explore what to say if a patient makes sexually suggestive remarks or hands their food tray to the only Black doctor in the room.
Boosting interprofessional collaboration and mutual support are also crucial. Wells LaRiviere, MD, PhD, now a first-year general surgery UC resident, still remembers one such lesson from his bootcamp last year. “A speaker was describing a patient who was becoming aggressive. The resident handling the call could have just ordered a sedative, but the speaker stressed the need to go stand with the nurse at the patient’s bedside, that it was important to be supportive to the nurse in a difficult situation.”
Mutter emphasizes another important skill for incoming residents: recognizing one’s own limitations. “As the knowledge base in medicine continues to explode, you can’t know everything,” she says. “So one crucial skill is to know [when and] how to seek help — and that it’s okay to ask for help even if you’re embarrassed.”
For LaRiviere, one of the bootcamp’s greatest benefits was a solidified sense of what it means to be a doctor. “I came away with an even stronger understanding that this isn’t just a job. It’s a mission,” he says.
Building a better bootcamp
While bootcamp directors are running these intense courses, they are also trying to better understand what’s working and what’s not.
So far, studies point to some successes. One survey of residents and fellows found higher self-reported preparedness among participants — 85% — compared to 70% of those who didn’t attend a bootcamp. Another study found that surgical program directors gave bootcamp participants higher marks on efficiency in intern duties than nonparticipants. Other studies are more mixed, such as one suggesting that bootcamp participants did not perform significantly better than nonparticipants. But Rustici and others say conducting research on bootcamps’ impact can be challenging, partly because intern performance is influenced by numerous factors such as their ability to adapt to working in a new environment.
Other efforts focus on better understanding bootcamps’ on-the-ground offerings. “Educators have been doing a lot of work in recent years to get a better sense of the content of courses, how they’re evolving, and the direction the field needs to take,” says Dorothy Andriole, MD, AAMC senior director of medical education research.
Already, TTR experts have made some crucial advances.
Rustici and colleagues came up with 37 skills all TTR bootcamps ought to cover. The consensus effort — which involved surveying more than 100 TTR educators, residency program directors, and residents — took two years. In January, another team published guidance on how to create a high-quality course, such as asking recent residents which skills they wish they had learned. Anyone who wants more direction can also attend a bootcamp for bootcamp directors offered by a consortium called Transition to Residency Course Educators .
But perhaps the most significant effort has been the consortium’s vetted compendium of curricula, available for free online in six different medical specialties. Three major surgical organizations also collaborated to produce bootcamp modules that schools can customize, with everything from pre-readings to model test questions.
Looking ahead, TTR educators hope to further enhance bootcamp trainings.
Amy Gonzalez, MD, who codirects the UTMB course, would like to see more personalized course schedules, so trainees can focus on skills they feel will most help them succeed. In fact, the UTMB course runs much like a conference, with students selecting from a menu of options. “We feel strongly that this approach makes it more impactful for students, and we believe individualizing is an important future direction for the field,” she says.
Mutter would like to see greater coordination between schools and residency programs, including increased sharing of information about students, based partly on bootcamp performance. “It can be tricky because we don’t want to bias programs, but I predict a lot of upcoming research will focus on how to hand off students well, to help residency directors know where interns need more support during the transition,” she says.
Meanwhile, Rustici says his colleagues remain highly committed to providing the best possible bootcamps. “Transition to Residency directors are passionate about this amazing opportunity we have to impact student development,” he says. “We are dedicated to helping them learn to deliver the kind of care we want all future patients to receive.”